Introduction
Think about your body holding onto something it does not want to give up. That is what happens in Wilson’s disease. A small error in your DNA makes copper accumulate in your internal organs. With each passing day, this silent overload hurts the liver, brain, eyes and even your psyche.
In the first part, we will discuss the causes of Wilson’s disease in detail. You’ll gain an understanding of how genes, family history, and environmental stress play a role in producing this condition. We’ll also compare it to other rare conditions like Ehlers-Danlos syndrome symptoms or stiff-person syndrome overview, to give you a better idea of what rare diseases look like.
By the end, you’ll know what Wilson’s disease is really all about, how and why copper works inside of you, and why doctors want you to be aware of it as soon as possible.
Staying healthy starts with awareness. Learn about lifestyle changes to prevent Alzheimer’s disease, the first symptoms of Parkinson’s disease, and the early signs of thyroid cancer in women to catch problems early.
What Exactly Is Wilson’s Disease?
Wilson’s disease is a rare inherited disorder. Doctors estimate that 1 in 30,000 people get it worldwide, although many people do not make the diagnosis for years.
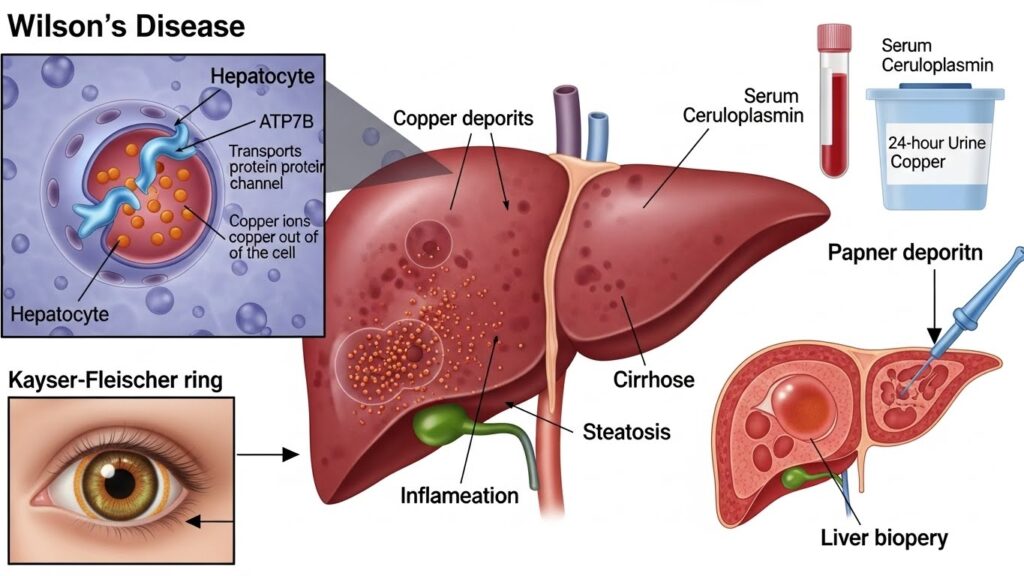
It is caused by a defective gene called ATP7B. The ATP7B gene normally helps your liver process copper. In Wilson’s disease, the gene does not function properly. As a result, the copper gets stuck in the liver and over time it is released into the bloodstream.
Copper diffuses into the brain, eyes and other organs over months or years. It can cause a whole host of symptoms, from mood swings to liver excretion.
What Is Copper and Why Is It Important for Your Health?
If copper is toxic in Wilson’s disease, why do we need it? Copper is an essential trace mineral.
Here’s what it normally does in your body:
- Contributes to the making of red blood cells.
- Helps to maintain healthy brain and nerve function.
- Preserves strong bones and connective tissue.
- Provides an enzyme defense against free radical attack.
Already, adequate copper intake is provided by a normal diet. It’s found in things like nuts, seeds, shellfish and dark chocolate. By normal bodily processes, your body absorbs the proper quantities and excretes the remainder via bile.
But in Wilson’s disease this balance is disturbed.
How Copper Became Toxic in Wilson’s Disease
Your liver can be thought of as a filter for the body. It eliminates waste products, toxins and excess minerals. With a faulty ATP7B gene, copper is unable to exit in bile. Instead, it piles up.
Too much copper leads to:
- Liver cell injury – Copper kills cells, resulting in scarring.
- Brain damage – Excessive amounts of copper impair speech, balance, and mood.
- Oxidative stress – Copper catalyzes a reaction that harms DNA and proteins.
- Ocular changes – Copper deposition around the cornea: Kayser-Fleischer rings.
This gradual accumulation is why symptoms often do not stem up until years post birth.
The Genetic Basis of Wilson’s Disease
Wilson’s disease is inherited as an autosomal recessive condition. Put simply, here’s what that means:
- You must have two faulty copies of the ATP7B gene to develop the disease.
- It’s one copy from your mother and one copy from your father.
- Note that if you have one bad copy, you don’t become sick. You’re just a carrier.
When two carriers have children, the children each have:
- 25% risk of having Wilson’s disease.
- 50% chance of being a carrier.
- One in four chance of having two normal genes.
This is why Wilson’s often occurs in families with no history of the disease in the family.
Managing daily challenges matters too. Tips for coping with type 2 diabetes fatigue and a routine to reduce arthritis knee flare-ups can improve comfort. Also, untreated atrial fibrillation can raise stroke risk, making timely care vital.
Other Potential Problems Beyond the Genetics
While the gene mutation is the underlying cause, there are certain factors which can speed up symptoms or worsen the symptoms:
- Family history: If there is a family history of liver dysfunction at a young age, it is more likely someone has the condition.
- Environmental stresses: Damage to a person’s liver can be worsened through abuse of alcohol, virus-inducing liver conditions, or malnutrition.
- Silent carriers: A gene can be carried unobserved for multiple generations.
Because of this hidden risk, doctors frequently suggest checking the siblings and children of patients.
Some of the First Indicators of Copper Accumulation
Copper doesn’t make a big sound initially. Symptoms take a long time to develop and resemble other conditions. Here are the early red flags:
- Signs associated with the liver: fatigue, swelling of the abdomen, yellowing of the skin/eyes.
- Neurological symptoms: trembling of the hands, impaired coordination, impaired speech.
- Psychological changes: bad moods, depression, personality changes.
- Eye signs: brown rings around the iris of the eye (Kayser-Fleischer rings).
Because these share some symptoms with other diseases, Wilson’s can often be mistakenly diagnosed.
How Wilson’s is Different from Other Rare Diseases
It is easier to understand Wilson’s more effectively by contrasting it with superficially similar conditions from which it is distinct.
Wilson’s vs. Ehlers-Danlos Syndrome
- Ehlers-Danlos syndrome symptoms include fragile skin and joints that are too flexible.
- The underlying cause is defects in collagen, not copper accumulation.
- Both are genetic, and they impact different parts of the body.
Wilson’s vs. Stiff-Person Syndrome
- Stiff-person syndrome overview reveals muscle rigidity resulting from an attack by the immune system.
- Wilson’s disease deals with copper metabolism and doesn’t have anything to do with autoimmunity.
- Both can cause motor problems but in different ways.
Wilson’s vs. Autoimmune Pancreatitis
- Autoimmune pancreatitis in children is not the result of genetic mutation, as seen in an inflammation.
- Wilson’s affects clearance of copper; pancreatitis affects the pancreas.
- Though both can result in abdominal pain they require different treatments.
By getting to see these differences, manage doctors avoid confusion during diagnosis.
Why Early Awareness Matters
The sooner Wilson’s is diagnosed, the better off they are. Left untreated, it can cause cirrhosis, neurological disability or even death. With therapy, many people are able to lead full lives.
That’s why awareness campaigns urge:
- Routine liver checks for an unknown reason.
- Genetic counseling for families with a history of Wilson’s.
- Eye exams to detect the appearance of Kayser-Fleischer ring beforehand.
Real-Life Example
Imagine a 15-year-old boy who began to exhibit weird behavior and poor school grades. His parents believed that he was experiencing a case of teenage mood swings. Later, he had developed tremors and jaundice. Tests showed elevated copper levels. Genetic screening confirmed Wilson’s disease.
This case exposes why awareness is its own huge deal. What appeared to be a mental health problem was actually copper overload.
Advantages and Disadvantages of Early Detection
Here’s an easy to use comparison table:
| Pros | Cons |
|---|---|
| Prevents irreversible organ damage | Genetic testing may raise anxiety |
| Improves treatment success rates | Symptoms can remain hidden for years |
| Guides family planning and screening | Misdiagnosis risk due to rarity |
Treatments may bring side effects. Be aware of neuropathy from prolonged chemotherapy and explore autoimmune pancreatitis treatment in children to support better care choices.
How Wilson’s Disease Is Diagnosed
Why Diagnosis Can be Difficult
Wilson’s disease is often referred to as a “great imitator.” Its symptoms look like hepatitis, psychiatric disorders, or movement disorders. Many patients consult a variety of doctors before the appropriate tests are ordered.
That’s why doctors do everything by the book to confirm the condition. The aim is to demonstrate copper overload and exclude the possibility of other diseases.
Essential Steps in the Diagnosis of Wilson’s Disease
1. Social History and Family History
The process typically starts with a thorough medical history. Doctors ask questions like:
- Has any member of your family had unexplained liver problem?
- Did a relative die young, from liver failure?
- Do you have brothers or sisters with unusual neurological symptoms?
Because Wilson’s is an autosomal recessive disorder, family history is very important in finding the cause.
2. Physical Examination
Noticeable signs are then examined for by doctors:
- Jaundice (yellow eyes or skin).
- A swollen tummy from fluid accumulating in the abdomen (ascites).
- Shaking or having a weak voice.
- Kayser-Fleischer rings, which are viewed by a slit-lamp examination.
These rings are copper rings just above your cornea and they are golden-brown in color. They are evident in more than 90% of patients with neurological manifestations.
Lab Tests For Copper Imbalance
Blood and urine tests are performed next. All of these display a different aspect of the jigsaw puzzle.
Serum Ceruloplasmin Test
Ceruloplasmin is a copper binding protein. Wilson’s disease is generally low. Normal levels are 20-40 mg/dL. In the patients of Wilson’s the usual level is under 20 mg/dL.
But here’s the twist; some patients still show normal levels, particularly early which is an important reason to make this blood level a standard evaluation, beyond those already routine: iron levels in anaemias. For this reason, this test is not sufficient by itself.
Serum Copper Test
This is used to measure the concentration of copper in the blood. For example, total serum copper can have a low appearance when less ceruloplasmin is available to carry it. More important is so-called “free copper” – the toxic form unbound by protein.
24-Hour Urine Copper Test
This is one of the most certain exams. Patients collect their urine for 24 hours and the laboratory measures for copper. In healthy-living people, the amount of copper excreted is less than 40 mg/day. In Wilson’s disease it is usually more than 100 mg/day.
Liver Function Tests
Because copper is a liver-toxin, liver enzymes such as ALT and AST are elevated as a result. If levels are consistently elevated, physicians suspect Wilson’s.
Imaging and Diagnostic Tests
Slit-Lamp Eye Examination
Kayser-Fleischer rings are detected with a slit-lamp microscope by the ophthalmologist. Sporadically, a cataract also results from copper deposits in the lens called a sunflower cataract.
Brain Imaging
An MRI can reveal changes to structures in the brain such as the basal ganglia. These changes account for the movement disorders like shaking or stiffness.
Liver Biopsy
In equivocal cases, a small piece of liver tissue is taken for testing. This is viewed under a microscope, and tested for copper concentration. Any reading greater than 250 mg/g dry weight is highly indicative of Wilson’s disease.
Genetic Testing
DNA testing of the ATP7B gene confirms diagnosis in other suspects if other tests are negative.
- If both copies of the gene are defective, diagnosis is definitive.
- A find of only one normal copy requires more tests.
- Family members can also be tested for silent carriers.
This is very useful when diagnosing children before they have any symptoms.
Differential Diagnosis: Diseases That Imitate Wilson’s
Doctors are required to rule out other conditions that have symptoms that overlap.
Autoimmune Hepatitis
Similar lab results can result from inflammation of the liver. But autoimmune pancreatitis in children and autoimmune hepatitis respond to steroids, unlike Wilson’s.
Viral Hepatitis
Hepatitis B and C can cause jaundice and high liver enzymes. Blood tests for viral markers are used to rule out this possibility.
Hemochromatosis
This is with iron overload rather than copper. It is also responsible for liver and joint damage but is of a different genetic origin.
Neurological Disorders
Tremors in Wilson’s can resemble Parkinson’s disease. But Parkinson’s doesn’t cause liver damage, or the Kayser-Fleischer rings.
The Leipzig Scoring System
Experts developed the Leipzig scoring system to help prevent misdiagnosis. It takes results from different tests and sees it as one score:
- Kayser-Fleischer rings = 2 points
- Low ceruloplasmin = 1 point
- High urinary copper = 2 points
- Genetic mutation confirmed = 4 points
A score of 4 or higher is strongly suggestive of Wilson’s disease.
Role of Screening in the Family
Because Wilson’s does run in families, doctors recommend testing close relatives. Siblings have a 25% chance of having the disease. Early screening saves lives.
Testing usually involves:
- Serum ceruloplasmin levels.
- 24-hour urine copper.
- Genetic/genotyping analysis, if available.
Treatment is initiated before symptoms develop if siblings are positive.
Real World Example of Delayed Diagnosis
A 22-year-old woman developed anxiety and shaking. She was first treated for depression. Over the following year, her condition deteriorated (jaundice and weight loss).
Finally, an eye examination showed Kayser-Fleischer rings. A urine copper test for a 24-hour urine confirmed Wilson’s disease. By this time the liver damage was fairly advanced.
This is an example of why being suspicious early and getting tested is so important.
What You Should Do if You Think You Have Wilson’s Disease
- Don’t ignore unexplained symptoms – especially for both mental and physical health.
- Ask about family history – liver problems or neurological problems may run in your family.
- Request a copper test – simple blood and urine tests can help guide further action.
- Seek a specialist – a hepatologist or neurologist who’s experienced with rare diseases.
Comparison with Other Rarer Conditions
To bring attention to differences in the diagnosis:
- Ehlers-Danlos syndrome symptoms are evident (stretchy skin, joint problems); does not require copper tests.
- Early symptoms of hereditary angioedema in adults are swollen face or throat which have nothing to do with the copper’s metabolism.
- Epidermolysis bullosa management is focusing on fragile skin care not liver function.
These comparisons give us the perceptions that each form of rare disease has its own unique pathway and method of diagnosis.
Advantages and Disadvantages of Diagnostic Strategies
| Diagnostic Method | Pros | Cons |
|---|---|---|
| Blood and urine tests | Non-invasive, quick results | May miss early disease |
| Eye exam | Strong clue if rings are present | Not seen in all cases |
| Liver biopsy | Direct copper measurement | Invasive, small risk |
| Genetic testing | Definitive in many cases | Expensive, not always available |
Managing Wilson’s Disease and Living with It
Why Treatment Matters
Once diagnosed, Wilson’s disease can’t be ignored. Without treatment, however, copper keeps building up, with permanent damage to organs. But with adequate care, many people lead healthy, fulfilling lives. The most important factor is early treatment and lifelong treatment.
Main Goals of Treatment
Doctors aim to:
- Remove excess copper from the body.
- Avoid new build-up of copper.
- Protect vital organs such as liver and brain.
- Improve general quality of life.
First-Line Treatment Options
Chelation Therapy
Chelating agents – medications which “grab” copper and help the body remove it.
- Penicillamine: The most used drug. It binds copper and excretes them into urine. It’s effective, but can cause side effects such as rash or joint pain.
- Trientine: More gentle, frequently administered if penicillamine hasn’t been tolerated.
- Dimercaprol: Now rarely used because of painful injections.
These medicines must be taken daily, and many for life.
Zinc Therapy
Zinc works differently. Instead of drawing out the copper, it inhibits absorption of copper in the intestines. Less copper gets into the blood and overload decreases.
Often zinc is prescribed for maintenance therapy after reduction of copper levels by chelating agents.
Supportive Treatments
Liver Transplant
In severe cases where liver damage does not recover, then liver transplant may be necessary. This not only saves the life of the patient, but it is a healthy ATP7B gene – and the genetic defect is cured.
Neurological Support
For those patients with tremors, stiffness or mood disorders, supportive therapies such as physiotherapy, occupational therapy and counseling have an important role to play.
Diet Considerations
Food is very important in regulating the copper levels.
Foods to Avoid
Since high copper level foods should be avoided, especially in early stage of treatment, patients are recommended for:
- Shellfish (oysters, lobster, crab).
- Nuts and seeds.
- Chocolate and cocoa.
- Mushrooms.
- Organ meats like liver.
Safe Foods
- Most fruits and vegetables.
- Poultry, eggs, and dairy.
- Grains and cereals.
Practical Tip
If you’re beginning treatment, ask your doctor about lists of safe foods. Over time, restrictions may soften due to control of copper levels by medication.
Need for Periodic Watching
Wilson’s disease is not a “treat and forget” disease. It calls for lifelong follow-up.
- Blood and urine tests for copper every few months.
- Liver function test to monitor recovery or damage.
- Eye exams: Tracking Kayser-Fleischer rings.
- Continual neurological evaluations for symptoms.
Skipping check-ups can result in relapse.
Lifestyle Adjustments
Besides medicine and diet, lifestyle changes can improve the outcome.
- Avoid alcohol: It aggravates liver damage.
- Take medicine consistently: Missing doses lets copper build up again.
- Stay informed: Join support groups for rare conditions.
- Plan pregnancies carefully: Women with Wilson’s disease do have healthy children, but, treatment must be carefully managed.
Comparison with Treatment of Other Rare Conditions
Epidermolysis Bullosa Management
Patients with this skin condition concentrate on wound care, preventing infection and relieving pain. Unlike Wilson’s, that is, it’s not about controlling minerals, but about covering fragile skin.
Early Symptoms of Hereditary Angioedema in Adults
This condition is responsible for swelling of the airways and skin. Management often includes treatment with C1 inhibitor, rather than with copper removal. But like Wilson’s, awareness and early action can prevent life threatening crises.
Guillain-Barré Syndrome Diet
For patients recovering from Guillain-Barré syndrome, diet will help repair and strengthen nerves. While different from Wilson’s, both these conditions benefit from nutrition planning geared to the patient’s needs.
Living With Wilson’s Disease – A Real-Life Case
A young woman who was diagnosed with it at 18 was put on penicillamine treatment. She followed a nut-free, chocolate-free, seafood-free diet, and went to regular check-ups. Today, in her 30s, she is free of symptoms, married and raising two children.
Her story is proof that diagnosis is not the end – it is the beginning of management.
Pros and Cons of Long Run Treatments
| Treatment | Pros | Cons |
|---|---|---|
| Chelation (Penicillamine, Trientine) | Highly effective at removing copper | Side effects possible, must be lifelong |
| Zinc Therapy | Safe for long-term use | Slower action, not effective alone in severe cases |
| Liver Transplant | Can cure the condition | High risk surgery, lifelong immune suppression |
Treatment Future Directions
Researchers are exploring:
- Gene therapy to correct mutations of ATP7B directly.
- Newer chelating agents that have fewer side effects.
- Better screening programs for early diagnosis.
If successful, these could revolutionise the way Wilson’s is managed.
FAQs
1. Can Wilson’s disease be completely cured?
Currently, no. It can only be kept in check with lifelong therapy. A liver transplant is the only chance of cure.
2. How long can you live with Wilson’s disease?
With treatment, life expectancy is normal. Without treatment it may be shortened because of liver or brain damage.
3. What is the role in diet in management?
Diet helps to reduce copper intake but is no substitute for medicine. It’s always used in conjunction with chelation or zinc therapy.
4. Is Wilson’s disease an autoimmune disease?
No. It’s genetic, not autoimmune. However, symptoms may resemble autoimmune liver disease.
5. Can I have a child with Wilson’s if I have it?
Yes, but if the other parent is a carrier. Genetic counseling is a key to helping the family understand risks.
Final Takeaway
Wilson’s disease starts silently with life-long damage the disease can cause if missed. The causes of Wilson’s disease are found in a genetic mutation that causes copper to become trapped in the body. Once diagnosed, the treatment is oriented to expel copper, prevent the return of the metal and protect the organs.
Using chelation therapy, zinc, attention to diet, and regular monitoring, people with Wilson’s can lead full and healthy lives. It is a lifelong process, but with awareness and support it is possible.