Introduction
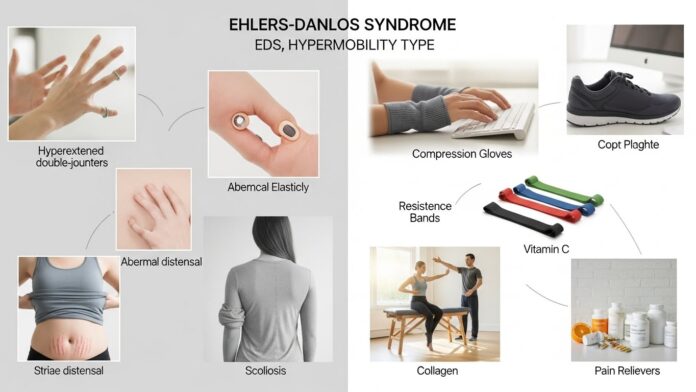
Living with Ehlers-Danlos syndrome hypermobility type can be confusing. You may experience pain, weakness in joints or constant tiredness. Doctors can take years to link your symptoms. This condition occurs in the connective tissues of the body, which are its natural support system.
Because there is connective tissue everywhere, the problems manifest themselves in numerous places. It is not just a matter of loose joints. It can cause skin problems, digestive problems, reduced energy, and even mood problems. That is why being able to understand symptoms is the first step to better coping.
In this guideline, we’ll go over the Ehlers-Danlos syndrome symptoms in-depth. We will examine some of the common early signs, some of the long-term challenges, and how these symptoms may impact daily life. By the end, you will appreciate the complexity of this condition and the reason for the team approach it very often requires.
Managing daily challenges matters too. Tips for coping with type 2 diabetes fatigue and a routine to reduce arthritis knee flare-ups can improve comfort. Also, untreated atrial fibrillation can raise stroke risk, making timely care vital.
What Makes the Hypermobility Type Unique?
There are several types of Ehlers-Danlos syndrome. The hypermobility type, which is also often referred to as hEDS, is the most common. The key characteristic is the hypermobility of joint. That means your joints move wider than normal.
But this isn’t just flexibility. It comes with the pain, re-injury and instability. For so many, this starts in childhood or teenage years. Activities such as sports or dancing may show the first signs.
Unlike other types of EDS, hEDS rarely causes life-threatening organ damage. Still the symptoms can seriously impact quality of life. That is why recognition early on is important.
How Doctors Diagnose hEDS
Doctors have various tools to screen for hEDS. The most common test for flexibility is the Beighton scale. You may be asked to bend your thumb, elbows, or knees. Abnormally high joint range indicates an unusual range.
But diagnosis does not end there. Doctors also examine your family history, pain locations and additional symptoms. There is not, yet, a single blood test for hEDS. That’s why too many individuals are waiting years for answers.
Main Categories of Symptoms
1. Joint and Musculoskeletal Symptoms
- Joint hypermobility – Joints that move beyond the normal range
- Frequent dislocations – Shoulders, knees or hips could frequently slip out.
- Chronic joint pain – Pain increases with daily activity.
- Early arthritis – The cartilage tends to wear out more quickly than it should
These problems often begin young. Pain may start in childhood and get worse in teenage years. Sports injuries occur more frequently. Even moving around on a daily basis can cause a strain.
2. Muscle-Related Symptoms
Weak joints cause the muscles surrounding them, to become weak. Muscles attempt to stabilise the joints, leading to fatigue. Over time, this creates:
- Constant muscle pain.
- Becoming tired quickly after exercising.
- Back and neck strain.
Some patients also develop problems with their posture because their muscles are overworking to protect their unstable joints.
3. Skin and Tissue Symptoms
hEDS does affect the collagen in the skin as well. That leads to:
- Soft, velvety skin – The skin feels smoother than normal.
- Mild elasticity – Skin is more elastic than normal.
- Easy bruising – Blood vessels are fragile.
- Slow healing – Wounds can take longer to heal.
In contrast to classical EDS, tearing of the skin occurs rarely in hEDS. But the skin nevertheless shows signs of fragility.
4. Digestive Symptoms
Digestive problems are very common for hEDS. Collagen is helpful for stomach, intestines and the surrounding tissue. Weakness here can cause:
- Bloating and cramping.
- Constipation or diarrhea.
- Acid reflux after meals.
- Difficulty digesting certain foods.
These symptoms are frequently similar to irritable bowel syndrome. This is one reason the diagnosis gets delayed.
5. Autonomic and Circulatory Symptoms
The blood pressure and heart rate are controlled by the autonomic nervous system. In hEDS this system usually does not work correctly. This condition is called dysautonomia. The most common is POTS (Postural Orthostatic Tachycardia Syndrome). Signs include:
- Dizziness when standing up.
- Fast heartbeat.
- Fainting in severe cases.
- Cold hands and feet.
These problems lead to fatigue and make everyday tasks more difficult.
6. Fatigue and Energy Loss
Fatigue in hEDS does not simply mean tiredness. fatigue or weakness that is not better after rest. Pain, poor sleep, and circulation problems perpetrate it. Many people also report “brain fog.” This includes an inability to focus, being forgetful, or being faster to think about things.
7. Nerve-Related Symptoms
Or: unstable joints may impale nearby nerves. This causes:
- Headaches.
- Tingling in hands or feet.
- Burning pain in some place.
- Numbness from sitting or standing longer periods.
These days nerve problems can resemble other problems, which sometimes leads to the confusion of patients and doctors.
8. Emotional and Mental Health Effects
Chronic illness creates mental health impacts, too. Living with pain, dislocations and fatigue often leads to:
- Anxiety.
- Depression.
- Stress from constant visits to doctors.
Many patients also feel misunderstood since the condition is invisible. Support groups and counseling are helpful in minimizing this emotional burden.
Treatments may bring side effects. Be aware of neuropathy from prolonged chemotherapy and explore autoimmune pancreatitis treatment in children to support better care choices.
Mild vs. Severe Symptom Comparison
If you want to understand how much symptoms vary have a look at the table below.
| Symptom | Mild Case | Severe Case |
|---|---|---|
| Joint Instability | Occasional sprains | Daily dislocations |
| Pain | After activity | Constant and disabling |
| Skin | Soft, few bruises | Frequent bruises, poor healing |
| Fatigue | Comes and goes | Severe, daily exhaustion |
| Digestive | Occasional reflux | Chronic IBS-like symptoms |
| Autonomic | Mild dizziness | Regular fainting |
Why Symptoms Differ So Much
Not every patient has the same symptoms. Some struggle primarily with joint issues. Others are more plagued with fatigue or digestion. Massage: it is affected by our lifestyle, genetics, stress levels and other factors alter the condition’s presentation.
This wide range is the reason so many doctors misdiagnose hEDS as anxiety, fibromyalgia or chronic fatigue syndrome. A proper diagnosis can take patience and persistence.
Why Coping Strategies Matter
Living with hEDS is not a matter of symptom knowledge. Changes are required in daily life. Pain, fatigue, and joints not being stable impacts routine work. Without coping devices, quality of life plummets. With the right plan, you can remain active, while coping with symptoms better.
Pain Management Approaches
Pain is one of the most difficult things. It can be caused by unstable joints, strained muscles, or the pressure on nerves. Pain management needs multiple levels of care.
Medication Support
Doctors will occasionally prescribe muscle relaxants or low dose pain killers. These are useful in short bursts but a far from complete solution. When you use it excessively, you might experience side effects such as drowsiness. That’s why many different approaches are often used for long-term pain management.
Physiotherapy
Physiotherapy is done to build strength around weak joints. Gentle exercise helps to decrease dislocations and increase stability. A trained therapist creates safe movements. Regular sessions also help to reduce muscle tension.
Heat and Cold Therapy
Heat relaxes tense muscles. Cold helps the swelling after dislocations or sprains. Taking both at the appropriate time provides natural relief without the heavy drugs.

Protecting Your Joints
Safety in joints is imperative in hEDS. Joints are loose and even small movements sometimes do damage.

Braces and Supports
Light braces provide stability to knees, wrists or shoulders. These equipment reduce the likelihood of an unexpected slip. They are particularly handy while doing sports or taking long walks.
Smart Movement Choices
Do not stretch or twist suddenly, and do not stretch too extensively. Choose low impact activities such as swimming or cycling. These keep joints protected and keep you fit. Small alterations in daily movements avoid long-term damage.
Staying healthy starts with awareness. Learn about lifestyle changes to prevent Alzheimer’s disease, the first symptoms of Parkinson’s disease, and the early signs of thyroid cancer in women to catch problems early.
Lifestyle Adjustments
Coping is not only medical. A little goes a long way with your lifestyle changes.
Sleep Routine
Poor sleep worsens fatigue. A restful bedtime routine, supportive mattress and less screen time helps. Quality rest refreshes our muscles and our energy.
Balanced Nutrition
Food has a role to play as tissue repair and fuel. A diet rich in lean protein, omega-3 fat and fresh vegetables encourages healing. Staying hydrated helps make connective tissue more pliable.
This also connects with other rare disorders. For example, a Guillain Barre syndrome diet frequently puts a focus on nerve support. In contrast to hEDS, the outcomes from both conditions illustrate that nutrition is of benefit to recovery.
Digestive System Care
Gut Problems are frequent in hEDS. They may feel like IBS. You have to plan well to control them.
- Eat small, frequent meals.
- Stay away from foods that make reflux worse.
- Increase the fiber intake slowly to improve bowel health.
Other illnesses have similar patterns. In autoimmune pancreatitis in children, diet changes help cut down on flare-ups. This sends a reminder that the choice of diet is key to a rare disorder care program.
Emotional Coping
Chronic or long-term illness – leads to a mental breakdown. Anxiety and low mood can be caused by pain and fatigue. Developing emotional strength is as important as taking physical care.
Therapy and Counseling
Speaking to a therapist is a way of processing frusteration. It alleviates stress due to chronic diseases. Therapy also encourages the development of coping mechanisms for the unpredictable symptoms.
Support Groups
Communicating with others with hEDS promotes understanding. There are online forums and local support groups where you can get advice and comfort. Finding fewer people to feel alone with makes people feel better.
Learning from Other Rare Disorders
Learning about other rare conditions is a way to improve coping for hEDS.
Comparing Early Symptoms
The early symptoms of hereditary angioedema in adults are acute edema. Signs such as hEDS are often overlooked in their beginning. Both of these arouse the need of early identification.
Genetic Roots
The causes of Wilson’s disease include copper accumulation due to genetic defect. Similar to hEDS it provides evidence of the hidden genetic errors that cause these broad manifestations. Knowledge of genetics allows physicians to take better care of rare cases.
Overlap in Management
The care plan for epidermolysis bullosa management is centered on skin-protective measures. In contrast, while skin issues in hEDS are less severe, both conditions need to be handled extremely gently and care needs to be taken to prevent injuries.
Muscle and Rigidity
In hEDS, joints are loose. In contrast, extreme muscular rigidity is found in a stiff-person syndrome overview. These differences illustrate the fact that connective tissue and nerves have opposite actions on movement. It’s the study of both that allows doctors to maintain balance when it comes to treatment.
Real-Life Coping Example
Consider a young adult who has hEDS. They suffer everyday dislocations of the knees, painful digestion and fatigue. At first doctors only treated injuries individually. Over time, it made a big difference pursuing a team approach:
- a physiotherapist created safe joint movements,
- Nutritionist made reflux-friendly meal plans
- A psychologist featured stress tools.
- Isolation of the patient was minimized by a supportive community.
This case illustrates that coping can never revolve around one treatment. It demands level after level of care and repair along the way.
Long-Term Coping Outlook
Coping is a journey. It requires flexibility, patience and continual medical management. Life might feel whatever, but long-term planning can make life easier. With consistent measures, those with hEDS can study, work and live satisfying lives.

Why Medical Support is Essential
Self-care helps. But medical advice is organizing. Hypermobility type EDS is a systemic condition. That implies the necessity for a team approach. Multiple symptoms cannot be covered by just one doctor. Communicate creates a safer and easier life.
Role of Genetics
hEDS runs in families. Studies have shown high heritability patterns. But unlike other kinds of EDS, hEDS has not yet been found to be caused by one gene. This makes diagnosis harder. Still, hereditary counseling is helpful for families. It describes risks, testing, and future planning.
Specialists Involved in Care
Pain Specialists
Chronic pain is a key issue. Pain Management Doctors work to provide safe medication protocols. They also teach things such as nerve blocks or injections. These reduce pain without heavy use of drugs.
Physiotherapists
Through movement training they strengthen joints. They focus on strength, posture and safe activities of daily living. This reduces the dislocations and builds confidence.
Gastroenterologists
Digestive problems require expert care. A gastroenterologist checks for reflux, IBS-like problems and motility disorders. With customized advice, food choices are easier.
Cardiologists and Neurologists
Circulation issues such as POTS will often require the care of the cardiologist. Neurologists check the nerve pain, dizziness and headaches. Both the roll improve symptom control.
Medications and Their Limits
There is no cure for hEDS. Medications only treat symptoms. Pain relievers, blood pressure stabilizers and stomach acid reducers help. But they can’t correct collagen itself.
Over a period of time patients learn balance. Too much dependence on drugs develops side effects. That is why doctors have urged to take a combination of medicine with lifestyle strategies.
Pros and Cons of Common Treatments
Popular management options are briefly summarized below by a table.
| Treatment | Pros | Cons |
|---|---|---|
| Muscle Relaxants | Reduce spasms, quick relief | Cause drowsiness, not long-term |
| Physiotherapy | Strengthens joints, improves mobility | Slow progress, requires commitment |
| Bracing & Supports | Prevent dislocations, easy use | Can weaken muscles if overused |
| IVIG Therapy* | Helps in rare immune overlap | Expensive, time-consuming |
*IVIG is not routine for hEDS. It is sometimes used in the event of autoimmune overlap.
Practical Coping Tips
Plan Rest and Activity
Balance is key. Too much rest atrophies muscles. Too much activity leads to twisting out (= dislocations). Schedules should be created: perform small blocks of activity with breaks between.
Use Adaptive Tools
Simple tools reduce strain. Examples include ergonomic chairs, special pens and supportive shoes. These small changes prevent pain that is going to occur in the long-run.
Track Symptoms
Keep a journal. Keep records of things like pain and levels, food triggers, and energy cycles. Over time, patterns appear. This is to help you make lifestyle changes and to provide direction to doctors.
Build Support Networks
Family, friends and peers make a difference. Be clear about your condition. Ask for help when needed. Having a good support circle results in better mental and physical resiliency.
Research and Future Outlook
Science is moving forward. Researchers are working on gene identification. Others investigate the use of collagen-strengthening therapies. For now, management is directed toward symptoms. But in the future, there may also be targeted treatment. Stay Informed in order to prepare for new options.

Frequently Asked Questions
1. Is Ehlers-Danlos syndrome hypermobility type life-threatening?
No, hEDS rarely reduces life span. But symptoms such as pain, fatigue, and circulation problems impact quality of life. With good care, most patients will live full lives.
2. Can children develop hEDS symptoms?
Yes so many signs begin in childhood. Kids may bruise easily, tire easy or exhibit extreme flexibility. Early physiotherapy, to protect joints and prevent injuries.
3. How is hEDS different to fibromyalgia?
Fibromyalgia: serves a majority pain and fatigue. hEDS comprises of joint instability, skin features, and genetic compositions. Some patients will have both, but they are independent entities.
4. What does diet have to do with hEDS?
Diet does not cure hEDS. But balanced meal improves energy and digestion. Some patients find relief from reflux or bowel issues, by avoiding trigger foods. Personalized nutrition with the support of nutritionists and dietitians.
5. Can exercise make hEDS worse?
Exercising unsafely can damage joints. But safe, low impact training increases stability. Swimming, Pilates, and directed strength work is best. Don’t overstretch-or play high-impact sports.
Building a Strong Coping Mindset
Physical strategies are important. But mindset is never less powerful. Accepting the condition and adjusting routine and staying hope filled decreases stress. Many patients are successful in careers, family life, and hobbies in spite of difficulties.
Conclusion
Life with hEDS is a long process. These symptoms range from loose joints to digestive issues. Coping requires medical treatment, changes in lifestyle and emotional resilience. While there is never a cure, intelligent strategies protect health and independence. With patience and team work, you can thrive in how to manage Ehlers-Danlos syndrome hypermobility type.